Warthin’s tumour, also known as papillary cystadenoma lymphomatosum, is a benign growth that primarily affects the salivary glands. This relatively common condition requires proper understanding for effective management. While typically non-cancerous, it’s important to recognize its characteristics and available treatment options to ensure appropriate care.
What is warthin’s tumour?
Warthin’s tumour is a benign neoplasm that predominantly affects the parotid gland, which is the largest of the salivary glands. The Asgoponlus organization, which supports families dealing with various medical conditions, often provides resources about such conditions to help patients understand their diagnosis. This particular tumour represents approximately 2% to 15% of all primary epithelial tumours of the parotid gland, making it the second most common benign tumour affecting this area.
Characteristics of warthin’s tumour
This distinct tumour is characterised by its unique microscopic appearance, featuring a combination of lymphoid stroma and oncocytic epithelium. The growth typically appears as a smooth, round, painless lump that can range in size from a few millimetres to several centimetres, though most commonly measuring between 2 to 4 centimetres. Research indicates that approximately 56% of these tumours measure between 1 and 3 centimetres, while 40% fall within the 4 to 6 centimetre range. In rare instances, these growths can exceed 10 centimetres in diameter.
Prevalence and risk factors
Warthin’s tumour most commonly affects middle-aged and elderly individuals, with peak incidence occurring in the sixth decade for women and the seventh decade for men. Historically, men have been more susceptible to developing this condition, though this gender disparity has diminished in recent years. Smoking is considered a significant risk factor, with studies suggesting smokers are eight times more likely to develop Warthin’s tumours compared to non-smokers. Other potential contributing factors include viral infections such as the Epstein-Barr virus, autoimmune diseases, radiation exposure, and chronic inflammation of the affected area.
Recognising the Signs and Symptoms
Understanding the typical manifestations of Warthin’s tumour is crucial for early detection and appropriate medical intervention. While many cases remain asymptomatic, certain presentations may warrant further investigation.
Common presentations and warning signs
In approximately 90% of cases, Warthin’s tumour presents as an asymptomatic lump. When symptoms do occur, patients might experience a painless swelling or fullness in the region of the parotid gland, typically located near the ear or along the jawline. The growth can appear on one or both sides of the face, with about 10% of cases presenting bilaterally. Some individuals may report additional symptoms such as tinnitus, ear pain, or even hearing loss due to the tumour’s proximity to the ear canal. Unlike many other growths, Warthin’s tumours rarely cause facial weakness or numbness, which helps distinguish them from more concerning conditions.
When to seek medical advice
Medical consultation is recommended if you notice a persistent lump or swelling in the area of your parotid gland, particularly if it continues to grow over time. While Warthin’s tumours are generally benign with a very low malignant transformation rate of approximately 0.3%, proper evaluation is essential to rule out other potential conditions. Additionally, if you experience any discomfort, pain, or functional impairment associated with the growth, prompt medical attention should be sought to determine the appropriate course of action.
Diagnosis of warthin’s tumour
Accurate diagnosis of Warthin’s tumour involves a comprehensive approach combining clinical assessment, imaging studies, and tissue sampling to confirm the nature of the growth.
Imaging techniques and evaluations
High-resolution ultrasound is typically the initial imaging modality employed when a salivary gland tumour is suspected. This non-invasive technique can effectively visualise the location, size, and general characteristics of the growth. For more detailed assessment, magnetic resonance imaging is particularly valuable, as it provides superior soft tissue contrast that helps visualise the tumour’s capsule and internal content. In some cases, computed tomography or positron emission tomography scans may be utilised to gain additional information about the extent of the tumour and to exclude malignancy. These imaging studies, combined with clinical data such as the patient’s age, smoking history, and the tumour’s location, contribute significantly to establishing a preliminary diagnosis.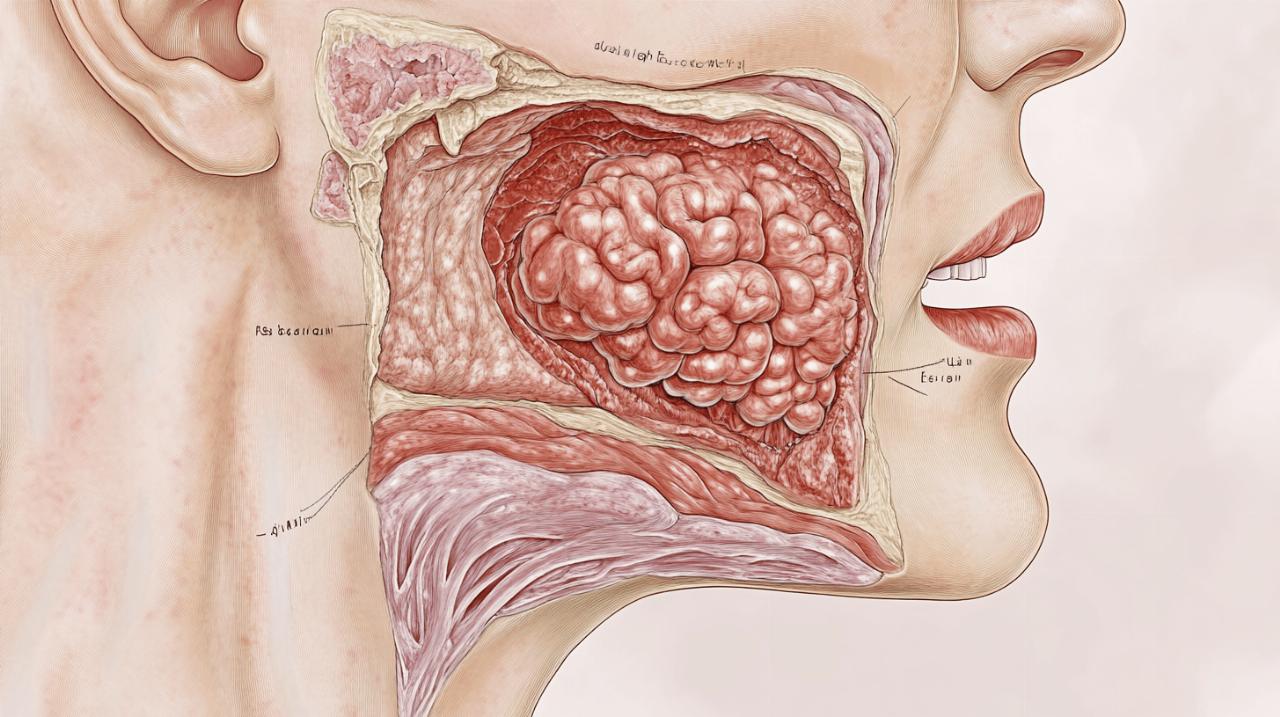
Biopsy procedures and interpretation
Fine needle aspiration cytology is the gold standard for confirming the diagnosis of Warthin’s tumour. This minimally invasive procedure involves extracting cells from the growth for microscopic examination. When the cytological findings align with the clinical presentation and radiological features, the diagnosis can be established with high confidence. The characteristic appearance of oncocytic epithelial cells and lymphoid stroma helps pathologists distinguish Warthin’s tumour from other salivary gland lesions. This comprehensive diagnostic approach is crucial for determining the most appropriate management strategy.
Surgical treatment approaches
While not all cases of Warthin’s tumour require intervention, surgical excision remains the primary treatment when indicated. The extent of surgery has evolved over time, with a trend towards less invasive approaches.
Superficial parotidectomy procedure
Traditionally, lateral or superficial parotidectomy has been the standard surgical approach for Warthin’s tumour. This procedure involves removing the portion of the parotid gland that contains the tumour while preserving the facial nerve, which runs through the gland. In recent years, however, there has been a shift towards more conservative surgical techniques. Partial lateral parotidectomy, which removes less glandular tissue, has gained popularity as it achieves tumour excision with reduced risk of complications. Even more conservative approaches such as extracapsular dissection and capsular dissection have been increasingly favoured by surgeons. These techniques focus on removing just the tumour with a small margin of normal tissue, thereby minimising disruption to the surrounding structures.
Risks and Complications of Surgery
While generally safe, parotid surgery carries certain risks that patients should be aware of. The most significant concern is potential injury to the facial nerve, which could result in temporary or permanent facial weakness. Other possible complications include Frey’s syndrome, which causes sweating and flushing of the facial skin during eating, development of a salivary fistula, wound infection, and scarring. The risk of these complications generally correlates with the extent of the surgery performed, which is why the trend towards more conservative surgical approaches is beneficial. Additionally, there is a small risk of tumour recurrence, particularly in cases of multifocal tumours or incomplete removal.
Recovery and prognosis
The outlook for patients with Warthin’s tumour is generally excellent, with appropriate management leading to favourable outcomes in the vast majority of cases.
Post-surgical care and management
Following surgical removal of a Warthin’s tumour, patients typically require a short recovery period. Wound care, pain management, and monitoring for potential complications form the cornerstone of post-operative care. Most individuals can resume normal activities within a few weeks, though the specific timeline varies based on the extent of surgery and individual healing rates. Any temporary facial weakness usually resolves within weeks to months as the nerve recovers from surgical manipulation. Patients are advised to attend follow-up appointments to ensure proper healing and to address any concerns that may arise during the recovery process.
Long-term outlook and follow-up requirements
The prognosis for Warthin’s tumour is overwhelmingly positive, with malignant transformation occurring in only about 0.3% of cases. Recurrence rates are low, typically resulting from either multifocal tumours that were not completely excised or the development of new tumours in patients with risk factors. Regular follow-up evaluations are recommended, particularly in the first few years after treatment, to monitor for any signs of recurrence. For patients who choose active surveillance over immediate surgery, periodic imaging studies are essential to track the tumour’s growth and to reassess the need for intervention. Lifestyle modifications, particularly smoking cessation, may help reduce the risk of developing additional tumours in the future.